This vivacast takes Tom on an epic battle,
Sundering his way through Oxygen Storage, crossing the Wheatstone Bridge, looking around corners with Fibre Optics and finally zapping everyone with Lasers.
Go and have a look at the VIE on your hospital site, channel your inner nerd! Good luck! Keep studying and Keep listening!
Article Spring Board
How is oxygen stored for medical use?
Medical oxygen is stored as a compressed gas in cylinders or as a liquid in cryogenic tanks, ensuring a continuous supply for therapeutic use.
What is oxygen
- Atomic number = 8
- Atomic weight 16 (15.9994)
- Valence = 2
- Molecular weight 32 (it floats about as two bound atoms)
- Medical O2 99% pure
- Fractional distillation of air compressed into liquid, (nitrogen and o2 boil out at different temps…)
- Colourless
- Critical Temperature -118DegC
- Boils at -183degC
- Pin Index 2, 5
- UK colour – white
- US colour = green
- Other Useful properties you will learn of later
- It is paramagnetic, ie drawn towards magnetic fields – has a
- It is not di polar (i.e there isnt an inclinication towards a slightly more positive and slightly more negative side, unlike water.
Vacuum Insulated Evapouators
Components:
- Thermos – vaccuum between an inner and outer tank
- Vapouriser/Evapourator to shift liquid to gas (allows for warming/volume)
- Warming – so hospital doesnt end up full of frozen pipes
- Gas extraction pipes from top of tank
- Liquid Extration pipes from bottom of tank – needs warming
- Weight Scale – Tank on hinge mechanism
- Valves/connectors to refill tank

Numbers
- High pressure 700KPa – 7 Bar
- Around -160 deg c
- Pressure release valve for the gas (at 1700KPa) (17 Bar)
- O2 pipeline hospital – 400KPa (4 Bar)
Chief Problems With Vacuum Insulated Evapourators
Pressure Drop
- If you pulled off all the gaseous O2 continuously,
- Oxygen shifts liquid > gas,
- Eventually the liquid, through latent heat of vapourisation would be so cool that not much would shift to gas
- Subsequently your oxygen supply would fail unless you started pulling off liquid and vapourising it yourself whilst waiting for the tank to warm up a jot.
Tank Over Heat
- Pressure release valve for the gas (at 1700KPa) –
- If the tank over heats it would overpressure
- Undergoing rapid unscheduled dissassembly, a pressure release valve dumps O2 instead of allowing this to happen. Think Gas Laws!
Safety Features
- Often an associated oxygen manifold of multiple oxygen tanks in two distinct groups (you can replace tanks while using the other) as a reserve.
- Or a secondary smaller tank adjacent to main.
Pipeline Safety Features
NIST – Non-Interchangeable Screw Threads on rear of anaesthetic machines.
Schrader collar to avoid wrong hose wrong line events for wall ports
Pipe colours – white for oxygen, blue for nitrous, black for med air, yellow suction Must be sure pipes inside the walls are correct too….


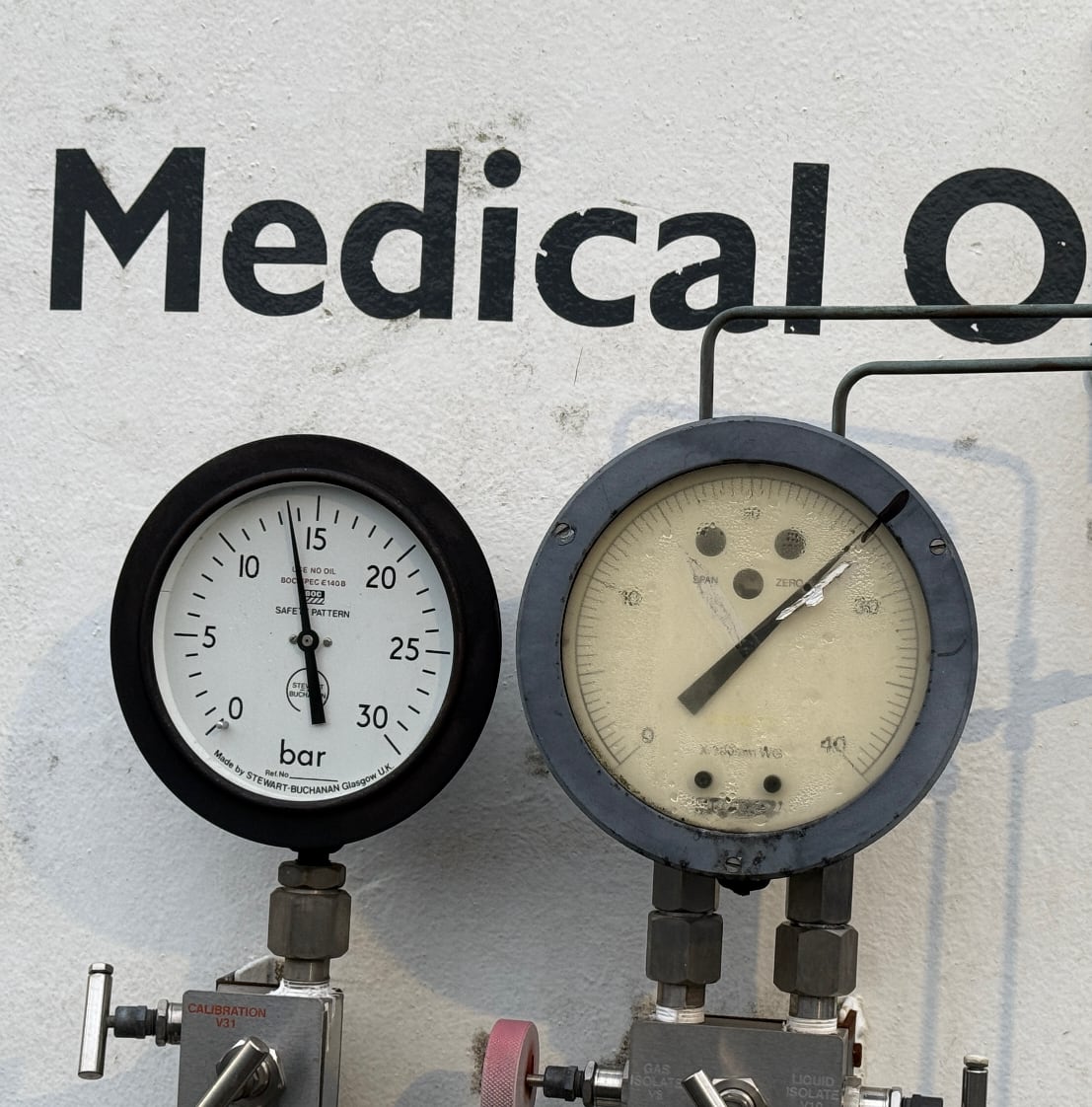
This VIE is at 14 Bar of pressure, I eat my words!
Oxygen concentrators in LTOT
The Chief mechanism is the Zeolite (hydrated aluminium silicates) molecular seives
- Seive retains nitrogen, yielding a greater concentration of oxygen (the other stuff in air remains)
- There are multiple columns of seives, as warming the column liberates nitrogen
- The colums are sequentially used, and warmed and the oxygen is pulled aside, the nitrogen off gases to atmosphere
- Argon is main remaining constituent
- Yields 95% o2
- Used for LTOT, but also field hospitals ETC
Pressure Measurement
Wheatstone bridge
- A cluser of resistors,
- Two pairs , in parralel with a volt meter between the two.
- There is a variable resistor controlled my microcontroller
- And the ‘measuring’ resistor which is:
- the device that senses the physical measurement target, in this case pressure
- for arterial lines – there is a piezo-resistive material that (one which alters its resistance dependent on the pressure applied
- It works on ‘null deflection’
- This means that the variable resistor alters its resistance in order to achieve a voltage difference across the two arms of the bridge of zero.
- By doing so it knows the resistance of the measured element and can infer signal from that put it through a micro-processor and provide a pressure wave reading.
Resistors are:
- an electrical component which regulates the flow of electrical current.
- Property = resistance measured in Ohms
Capacitors are:
- an electrical component which stores an electric charge as an ‘electrostatic field’
- Made up of two conductive materials seperated by an insulator, the so called dielectric
- Property = capacitance – Measured in Farads
Arterial Line Error Mechanisms
Damping
Anything that absorbs the pressure wave, ie and air bubble that takes some of the oomph/energy out of the pressure wave, springy tubing instead of stiff tubing – excessively long lines etc. You will see this in a feckless rounded wave-form that yields an accurate MAP but a narrower and incorrect measurement of sys/dia (ie 90/70 instead of 110/65) A clot in the line just messes up all the readings, if entirely blocked may read 0 or 300 (ie the pressure in the bag that it has delivered into the line)
Resonance
Like the resonance cascade of half life 1 yore, resonance is the amplification of a signal by a ‘system’ – Resonance Cascade
That could be soldiers marching in unison across a suspension bridge – hitting the bridges frequency and making it bounce to pieces (marching soldiers are allowed to break step when crossing a bridge for this reason)
Or in the case of measuring an arterial pressure pulse, if the system began bouncing neatly a heart rate of 60 against its ends up and down the tubing and each pulse added to the wave ricocheting up and down, it would not do a great job of reading blood pressure.
As such the natural frequency of the system doing the measuring, must be significantly different from the range of frequncies of the system it is trying to measure.
Im sure you’ve made waves in a pool, and figured out a way to time the wave making so that the waves climb in height, timing te swing of your legs on a swing is a similar ‘amplification’ of the waveform that is you swinging back and forth.
The governing factors for a systems natural frequency are:
- Directly related to the diameter
- Inversely related to the square of the systems compliance
- Inversely related to the square of the tubing length
- Inversley related to the square of the fluid density int he system
Of note, we could sit here and think, well the range of frequency in an arterial system is just min max hr (0-240) this would be up to 4hz (240/60) if were doing all of human life/non life. ) but that fails to realise that the arterial pressure waveform is a composite of multiple underlying waves all added up, and these have differing frequencies too. So the natural frequency of the arterial line kit is well in excess of this 4Hz.
CO monitoring
Breaks down the arterial line wave form into its component waveforms.
Much like a P wave can hide inside a QRS complex in an ECG with 3rd degree heart block. There are multiple pressure waves traversing the arterial system and there additive and subtractive effects yield the summative waveform seen on an arterial line trace (see Deranged Physiology #the hero we needed Dr A Yartsev)
Only some of these wave forms define cardiac output, and as such breaking it apart allows the calculation of the Area under the curve of the bit we are interested in and thus the stroke volume from which we can calculate cardiac output.
Lasers
Light Amplification by Stimulated Emission of Radiation
- Properties: Collimated – Photons in parallel
- MonoChromatic – All of the same wavelength
- Coherent – all in the same phase as one another
Lasing mediums
- Ruby – 694nm. — Red — Eyeball PhotoCoag
- Nd:YAG -1064nm. — infrared. — Cauterize and cut – ENT
- CO2 – 10600nm. — infrared — Laryngeal mucosa
- Argon 480-515nm — blue-green — Eyeballs and port wine birth marks
How it works
- Flashing light
- into a lasing medium in a compartment with mirrors on all sides
- one mirror has an optional opening in it.
- Enough light enters to excite the electrons of the lasing medium
- As these electrons decay back to a less excitable state they release energy in the form of photons, and these are all of the same nature. These photons knock into other jazzed up electrons
- Once enough electrons are jazzed up and kicking out photons and knocking into their mates there is an awful lot of photons that have the same properties bouncing around.
How do these rowdy electrons get out?
Either through a mirror which reflects 95% back into the medium or a ‘brewsters window’ which will only let out polarised light out.
Laser safety
- Locks on doors
- Eye protection
- Designated safety officer
- Kit to douse airway fires
- COETT in airway laser surgery that wont melt
- 2 cuffed saline filled coetts
Check out the laser classification – therapeutic lasers are typically class 4 (the most powerful type)
Fibre optics
How do they work?
Glass fibre 20 microns thick, made up of two different types of glass, with a slightly differing refractive index.
These two materials with diff index trigger refraction as the light interfaces across that material change.
With sufficiently sensible choices of material, the light traveling along this fibre is bounced back inside the fibre entirely – so called : Total Internal Reflection.
Light must be introduced into this fibre at an approrpriate angle, generally speaking if it enters too steeply / cross ways against the longitudinal axis of the fibre, then it will fail to start ricochetting down the fibre.
This angle is called the critical angle
Components of a fibre optic system
- Light source
- Fibres that conduct the light source
- Recieving fibres to conduct light (and the image) back
- Lens (think rigid ENT scope type action) / light sensing apparatus (you want the image on a screen instead)
And then depending on question they might be asking about the other elements of a Bronchoscope - Suction/irrigation port
- Control wires to direct tip
References
“Thanks for listening guys… Every day you are getting better at this. Take it day by day, don’t overcook yourself, don’t freak out, and keep studying!”
Podcast Information & Support
Support the Show
Contact & Feedback
- Comments: Share your clinical experiences and ask questions!
- Corrections: Help us improve accuracy and clarity
Follow GasGasGas On
- BlueSky:Gas Gas Gas (@gasgasgaspodcast.bsky.social)
- X / Twitter: GasGasGasFRCA (@GasGasGasFRCA) / X
- FaceBook: Facebook – Gas Gas Gas
- InstaGram: GasGasGas
Transcript
Physics & Equipment – Oxygen, Arterial Lines, Resonance & Fibre Optics
Introduction
00:00-00:30 Hello and welcome to Gas Gas Gas, the podcast that covers the FRCA primary exam. We’re going to fit into your day and give you as much of your life back as you could possibly imagine. Listen to us on your commute, in the gym, in the shower, or when ironing your scrubs. Expect facts, concepts, model answers and the odd tangent. Check out the show notes for all the detail, and remember to follow the show so that you never miss an episode.
Physics and Equipment Viva
01:01-01:04 Time for your physics and equipment viva. Are you ready for action?
What is Oxygen?
01:04-02:15
Oxygen is a gas composed of two covalently bonded oxygen atoms, found at approximately 21% concentration in atmospheric air. It has a critical temperature of around -118°C, placing it above its critical temperature at standard temperature and pressure conditions. Oxygen is essential for biological processes in humans, particularly for cellular energy generation through various metabolic processes.
Hospital Oxygen Storage Systems
02:15-05:18
Vacuum Insulated Evaporators (VIEs)
Oxygen can be stored in two main ways in hospitals:
1 Portable cylinders
2 Large oxygen manifold storage containers (VIEs)
⠀VIE Specifications:
- Temperature: Kept below oxygen’s critical temperature (typically -150°C to -180°C)
- Pressure: Approximately 700 kilopascals (7 bar), potentially up to 10 bar
- Pipeline pressure: Reduced to approximately 4 atmospheres through pressure-reducing valves
- Safety features: Pressure blow-off valve prevents unsafe pressure levels during system problems or high temperatures
- Insulation: Vacuum container prevents heat entry for efficiency
⠀Quantity measurement: Only reliable method is weighing the entire container, providing accurate measurement regardless of oxygen state within the container.
Manifolds vs. VIEs
Manifold: System connecting multiple gas containers/cylinders for efficient transport from multiple sources VIE: Single large container within a vacuum system
Backup systems: Manifolds often provide backup for VIEs in case of malfunction.
Temperature-Related Issues
Too hot: Pressure blow-off valves activate Too cold: System pressures drop, impairing oxygen supply; heating elements maintain adequate pressure in various system components
Cylinder vs. VIE Supply Differences
05:07-05:44
VIE advantages:
- Practically unlimited supply
- Constant pressure delivery (~4 atmospheres)
⠀Cylinder characteristics:
- Limited volume delivery
- Pressure decreases as oxygen volume decreases (unless processed)
⠀Gas Pipeline Safety Features
05:44-07:20
Colour Coding
- Air: Yellow
- Nitrous oxide: Royal blue
- Oxygen: White
⠀Schrader Valve System
Non-interchangeable colour-coded connections prevent accidental gas line mix-ups (e.g., cannot attach oxygen line to nitrous oxide outlet).
Pin Index System (Cylinders)
5-pin arrangement with female connectors that only fit correct gas types:
- Most connections: Include pin number 5
- Oxygen: Pins 2 and 5 (2 atoms in oxygen molecule)
- Nitrous oxide: Pins 3 and 5 (3 atoms in nitrous oxide molecule)
⠀Home Oxygen Therapy
07:26-08:14
Occasional use: Oxygen cylinders Long-term therapy: Oxygen concentrators
- Concentrates oxygen from atmosphere
- Delivers on-demand oxygen
- Avoids safety concerns of storing pressurised high-volume oxygen
- Safety consideration: Can create supernormal oxygen concentrations in enclosed spaces with associated fire risk
⠀Wheatstone Bridge
08:18-09:26
A sensing circuit designed to determine exact resistance of variable resistance sensors by arranging resistors in parallel within a circuit.
Mechanism: Modify resistance of known adjustable resistor until voltage between the two bridge arms reaches zero volts, determining the unknown sensor resistance.
Applications:
- Temperature sensing (thermocouple devices)
- Arterial line pressure measurement
- Widely used in sensing systems
⠀Key relationship: V = IR, therefore R = V/I
Resistors vs. Capacitors
09:52-10:39
Resistors
Resist electrical current flow constantly over time.
Capacitors
Structure: Two non-conducting surfaces in close proximity with potential difference applied across them Function: Causes electron build-up on one side compared to the other, which can then be released Capacitance relationship: Higher capacitance = higher electron storage = higher energy release potential
Units:
- Resistance: Ohms
- Capacitance: Farads
⠀Arterial Line Accuracy Factors
11:07-12:01
Beyond electrical circuits, signal accuracy depends on the initial signal quality:
Damping Causes
- Air in arterial line (compressible vs. fluid)
- Excessive tubing length dampens signal
- Under-damping causes noise and inaccurate readings
- Very short lines or transducer faults
⠀Resonance in Arterial Line Systems
12:01-13:16
Resonance definition: System’s capacity to vibrate consistently with the measured signal, amplifying and distorting it.
Analogy: Like swinging legs on a swing at the right timing – each correctly timed movement increases amplitude.
Arterial line context: Measuring heart rate, but arterial waveforms contain multiple other waves. Natural frequency matching between measuring system and measured signal creates resonance.
Governing factors:
- Diameter of measuring system
- Compliance of measuring system
- Length of tubing
- Fluid density within measuring system
⠀Cardiac Output Measurement via Arterial Lines
13:28-14:32
Basic formula: Cardiac output = stroke volume × heart rate
Area under the curve method: Arterial line trace area provides cardiac output guidance through Fourier transformation, breaking waveforms into component sine waves for accurate area calculation.
Difficult Airway Equipment
15:11-16:23
For absolutely necessary intubation in very difficult airways:
Primary equipment options:
- Videolaryngoscope
- Fibre-optic equipment
⠀Additional considerations: Complete difficult airway trolley with various adjuncts (airways, tubes, rescue devices).
Fibre-Optic Scope Components
16:25-17:47
Components:
1 Light source
2 Fibre-optic bundle inserted into patient
3 Viewing system: Either lens (older scopes) or digital display (modern scopes) showing image from distal end
⠀How Fibre-Optic Fibres Work
Structure: Many small glass fibres with radius small enough to induce total internal reflection
Mechanism: Light entering the fibre reflects internally at any point within the circular fibre, preventing lateral exit and ensuring light travels to the tube’s end where the image is created.
Fibre specifications:
- Core: Glass with protective polymer around outside
- Thickness: 10 microns to several hundred microns depending on application
- Refractive index: Cladding approximately 1% less refractive than core glass
- Critical angle: Light must enter at correct angle along fibre axis for total internal reflection journey
⠀Light Sources: Fibre-Optic vs. Laser
19:27-20:45
Laser Light Properties
Characteristics: Collimated, monochromatic, non-divergent, and coherent (in-phase)
LASER acronym: Light Amplification by Stimulated Emission of Radiation
Process:
1 Photon absorption by electrons → excited state (higher energy levels)
2 Second photon absorption → electron drops energy level
3 Releases two identical photons in phase
4 Chain reaction in lasing medium produces many in-phase photons
5 Ejection through partially silvered mirror in single direction
⠀Laser Types and Applications
Carbon dioxide lasers:
- Highest frequency and energy
- Tissue cutting and haemostasis through cauterisation
⠀Argon lasers:
- Slightly lower energy
- Retinal surgery applications
- Tissue ablation and haemostasis
⠀Ruby lasers:
- Lower energy levels
- Hair removal and tattoo removal
⠀Laser Safety Management
21:47-22:56
Personnel Safety
Eye protection: Safety goggles mandatory for all theatre staff (retina most susceptible) Access control:
- Door signs or preferably locking systems
- Internal admission only at appropriate safe times
⠀Fire Safety
Heat source considerations: Potential fuel and oxygen availability Precautions:
- Damp swabs around surgical field
- Laser-compatible endotracheal tubes with two saline-filled cuffs for airway surgery
- Specialised laser-resistant equipment
⠀

Leave a Reply